Orbital Fractures
Trauma to the upper face frequently results in fractures of the internal orbit. These may occur as isolated blowouts or associated with more complex adjacent facial fractures. The range of potential injuries to the internal orbit may vary from a small orbital floor defect to destruction of all four walls. Despite this potential for wide variation of internal orbital fractures, there are basic principles that can be applied to aid in diagnosis and treatment. The bony orbits play a vital role in maintaining normal function and aesthetics of the eyes. Accurate realignment or anatomic reconstruction of the bony orbit is essential to maintain normal function and appearance.
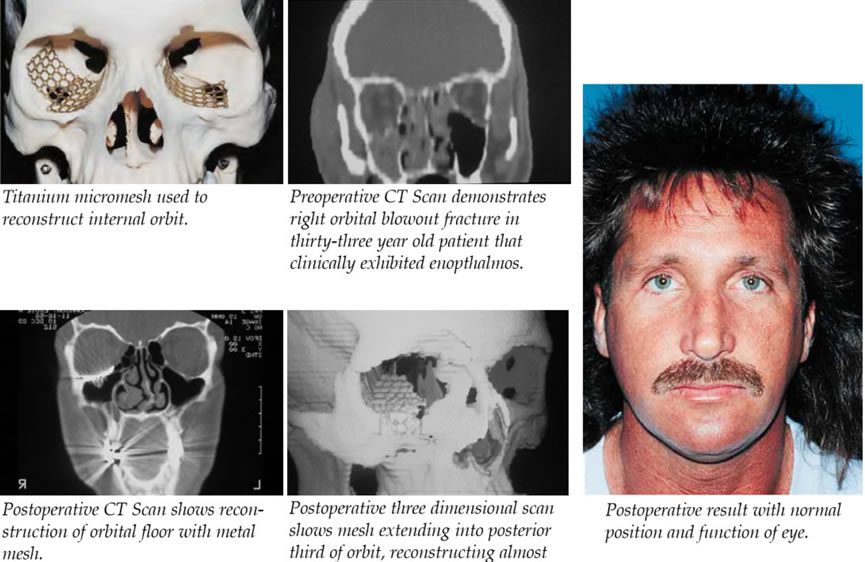
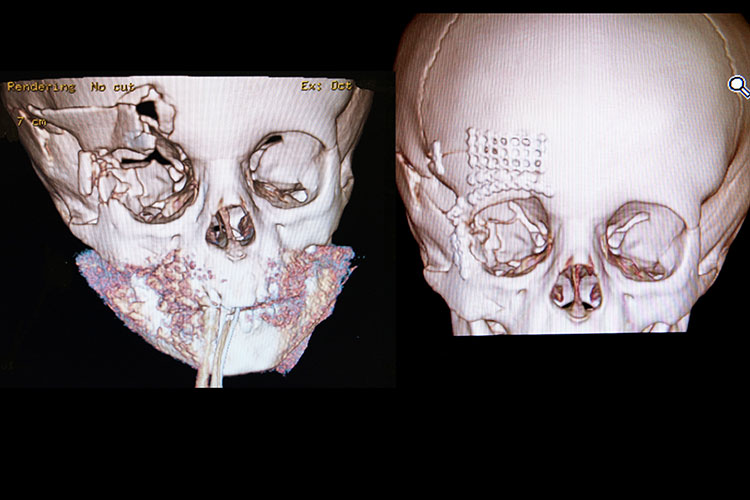
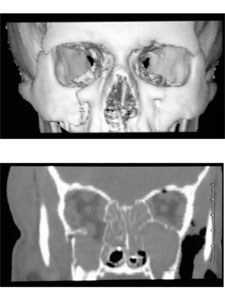
number of advances have been made in the past 10 to 15 years in the diagnosis and treatment of internal orbital fractures. The computerized tomographic (CT) scan has dramatically enhanced the surgeons ability to diagnose and determine the extent of the internal orbital fractures. Three-dimensional scans may even further enhance this radiographic evaluation. With the development of the field of craniofacial surgery, surgical techniques have also significantly improved in this area. These techniques have allowed extended exposure of the fractures, which greatly facilitates assessment and treatment of orbital injuries. Better exposure allows more precise reduction and rigid stabilization of the fractures. The other major advancement in orbital surgery has been the use of rigid fixation to provide a stable internal orbital reconstruction.
The use of mini- or microplates and metal meshes in combination with bone grafts has also improved stabilization and enhanced the healing of orbital fractures.
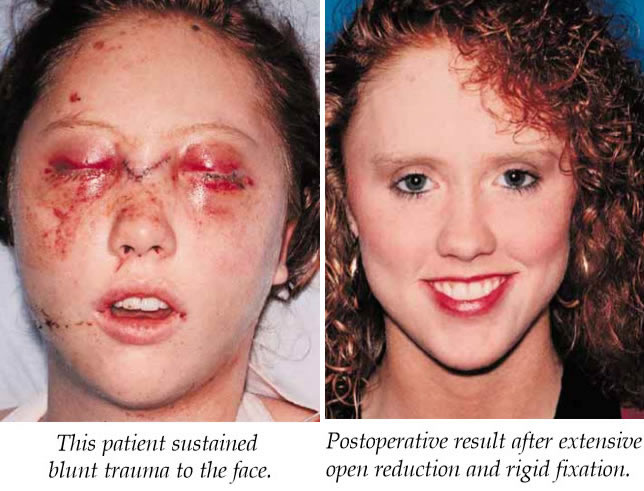
The recommended treatment of these injuries varies greatly in the literature with the best method of reconstruction remaining controversial. Surgical treatment has ranged from packing of the maxillary antrum to total orbital reconstruction with autogenous or synthetic materials. Accurate anatomic reconstruction is essential to restore function and appearance of the eye.

Because most of the bone of the internal orbit is thin and weak, it is frequently difficult to reduce and adequately stabilize without the use of autogenous or alloplastic materials.
Autogenous bone grafts have been the material most often used by craniomaxillofacial surgeons for reconstruction of the internal orbit. Split calvarial bone has gained popularity because of its low rate of infection and decreased resorption. Other autogenous materials that have been used include iliac bone, split rib, and cartilage. Resorption may be a problem with the use of autogenous bone. Each of these materials also requires a donor area, although donor site morbidity is usually very small.

A variety of alloplastic material such as silicone, teflon, tantalum mesh, polyethylene, and methyl methacrylate have been used for orbital reconstruction. The primary concern with the use of alloplastic material has been the risk of infection with extrusion. The metal miniplates systems have been very successful in the treatment of facial fractures. These techniques of rigid fixation using metal meshes have also been applied successfully to the treatment of internal orbital fractures. In our experience of reconstructing over 300 internal orbital fractures with metal mesh, we have found this technique to be both safe and effective with no infections as a result of using metal mesh.


The goal of surgical treatment of blowout fractures is to replace orbital contents back into the bony orbit and to restore normal orbital volume and shape. The best method of reconstruction of internal orbital fractures remains controversial. A number of techniques have been described using autogenous grafts or alloplastic materials. We have had good success with the use of metal mesh alone, without bone grafts, for the reconstruction in internal orbital defects. This micromesh is our preference when alloplastic material is used. It is rigid yet malleable and can provide excellent orbital support for large defects, particularly in the posterior aspect of the orbit. This is important, since accurate anatomic reconstruction of both orbital shape and volume is crucial to obtain the best possible results.
Significant advancements have been made in the evaluation and treatment of internal orbital fractures. CT has greatly enhanced our ability to identify the exact location and extent of destruction of internal orbital fractures. Early operative intervention combined with wide exposure, meticulous reduction, and rigid fixation has significantly enhanced the treatment of internal orbital fractures.